Daily Oral Hygiene Routine: Tips for Keeping Your Mouth Healthy
Maintaining good oral hygiene is essential for overall health. A healthy mouth allows you to speak, smile, and eat properly, preventing many dental and systemic diseases. This comprehensive guide provides tips for an effective daily oral hygiene routine to keep your mouth healthy and your smile bright.
The Importance of Oral Hygiene
Oral hygiene is more than just having white teeth and fresh breath. It involves caring for all aspects of the mouth, including teeth, gums, and tongue, to prevent dental problems like cavities, gum disease, and bad breath. Good oral hygiene is crucial because it can also impact overall health. Poor oral hygiene can lead to infections that may spread to other body parts, contributing to conditions such as heart disease, diabetes, and respiratory issues.
Daily Oral Hygiene Routine
A consistent daily oral hygiene routine is the foundation of a healthy mouth. Here are essential steps to incorporate into your routine:
1. Brushing Your Teeth
Brushing your teeth twice daily, in the morning and before bed, is crucial; this daily regimen helps remove plaque, a sticky film of bacteria that forms on your teeth and gums. Here are some tips for effective brushing:
Use the Right Toothbrush
Choose a toothbrush with soft bristles to avoid damaging your gums and enamel. Electric toothbrushes can be more effective in removing plaque than manual ones.
Use Fluoride Toothpaste
Fluoride helps strengthen tooth enamel and prevent decay. Choose a toothpaste with fluoride to maximize protection.
Proper Brushing Technique
Hold your toothbrush at a 45-degree angle to your gums and use gentle, circular motions. Brush all surfaces of your teeth, including the front, back, and chewing surfaces. Don’t forget to brush your tongue to remove bacteria and freshen your breath.
Brush for Two Minutes
Brush your teeth for at least two minutes to ensure you clean every part of your mouth thoroughly.
2. Flossing Daily
Flossing is essential for removing plaque and food particles between your teeth and under the gumline, where your toothbrush can’t reach. Here’s how to floss effectively:
Use Enough Floss
Break off about 18 inches of floss and wind most of it around each middle finger, leaving an inch or two to work with.
Gentle Technique
Gently slide the floss between your teeth. Curve it into a C shape against the side of each tooth and slide it under the gumline. Use a clean section of floss for each tooth.
Floss Regularly
Make flossing a daily habit to maintain healthy gums and prevent cavities.
3. Using Mouthwash
Mouthwash can be a beneficial addition to your oral hygiene routine. It helps reduce bacteria in your mouth, freshens your breath, and can help prevent gum disease. Here are some tips for using mouthwash:
Choose the Right Mouthwash
Look for a mouthwash containing fluoride to fight plaque and gingivitis.
Use Correctly
Pour the recommended amount of mouthwash into a cup, swish it around in your mouth for 30 seconds, and then spit it out. Avoid eating or drinking for 30 minutes after using mouthwash.
4. Cleaning Your Tongue
Your tongue can harbor bacteria that contribute to bad breath and plaque buildup. Cleaning your tongue is an essential part of oral hygiene. Here’s how to do it:
Use a Tongue Scraper
A tongue scraper removes bacteria and debris from your tongue. Gently scrape from the back to the front of your tongue.
Use Your Toothbrush
If you don’t have a tongue scraper, gently brush your tongue with your toothbrush.
5. Staying Hydrated
Drinking water throughout the day helps wash away food particles and bacteria, keeping your mouth clean. Staying hydrated also promotes saliva production, which is essential for neutralizing acids and protecting teeth from decay.

6. Eating a Balanced Diet
A healthy diet plays a significant role in maintaining oral health. Foods rich in vitamins and minerals, particularly calcium and vitamin D, support strong teeth and gums. Here are some dietary tips for oral health:
Limit Sugary Foods and Drinks
Sugar contributes to tooth decay by feeding harmful bacteria in your mouth. Limit your intake of sugary snacks and beverages.
Eat Crunchy Fruits and Vegetables
Foods like apples, carrots, and celery help clean your teeth as you eat them and stimulate saliva production.
Include Dairy Products
Milk, cheese, and yogurt are high in calcium and phosphates, which help strengthen tooth enamel.
7. Regular Dental Check-Ups
Regular visits to your dentist are crucial for maintaining oral health. Dentists can detect and treat issues before they become severe. Aim to visit your dentist every six months for a check-up and professional cleaning. During these visits:
Professional Cleaning
A dental hygienist will clean your teeth, removing plaque and tartar buildup you can’t remove at home.
Dental Examination
Your dentist will examine your teeth, gums, and mouth for any signs of problems such as cavities, gum disease, or oral cancer.
X-Rays
Your dentist may take X-rays to check for issues that aren’t visible during the examination, such as cavities between teeth or bone loss.
8. Avoiding Tobacco Products
Tobacco use is detrimental to oral health. It can cause gum disease, tooth decay, and oral cancer. Avoiding tobacco products is one of the best ways to protect your mouth and overall health.
Five Advanced Oral Care Tips
Beyond the basics, incorporating advanced oral care tips can further enhance your oral hygiene routine:
1. Using Interdental Brushes
Interdental brushes are small brushes designed to clean between your teeth and around braces, bridges, and implants. They can be more effective than floss for some people, especially those with wider spaces between their teeth or dental appliances that make flossing difficult. Use them daily to remove plaque and food particles from hard-to-reach areas, reducing the risk of gum disease and cavities. Additionally, these brushes come in various sizes, so you can find the one that fits your needs for optimal cleaning.
2. Oil Pulling
Oil pulling is an ancient practice that involves swishing oil (such as coconut oil) in your mouth for 15-20 minutes. This practice is believed to reduce bacteria, whiten teeth, and promote oral health. While not a replacement for brushing and flossing, it can be an additional step in your oral hygiene routine. The oil pulls toxins from the mouth and gums; some find it helps with bad breath and reduces inflammation. Including oil pulling in your daily routine may enhance oral hygiene and provide extra protection against dental issues.
3. Choosing the Right Dental Products
When selecting dental care products, choosing ones that meet your specific needs is important. For toothpaste, opt for a variety that contains fluoride to help strengthen enamel and prevent decay, and consider additional benefits like whitening or sensitivity relief based on your preferences. Similarly, select a mouthwash that addresses your concerns, whether for fresh breath, anti-cavity protection, or gum health. Several options are available for floss, including waxed, unwaxed, flavored floss, and floss picks. Choose the type that you find most comfortable and effective for your oral hygiene routine.
4. Managing Dry Mouth
Staying hydrated is essential for maintaining oral health, so drink plenty of water throughout the day to help wash away food particles and bacteria. Chewing sugar-free gum can also be beneficial, as it stimulates saliva production, which is crucial for neutralizing acids and protecting your teeth. A humidifier, especially during sleep, can add moisture to the air and alleviate dry mouth symptoms. Additionally, try to avoid alcohol and caffeine, as these substances can exacerbate dry mouth and contribute to dehydration.

5. Treating Sensitive Teeth
To manage tooth sensitivity, consider using desensitizing toothpaste, which contains compounds that help block the transmission of sensation from the tooth surface to the nerve, providing relief from discomfort. Additionally, avoid acidic foods and beverages, such as citrus fruits, sodas, and vinegar-based products, as they can erode enamel and increase sensitivity. Use a soft-bristled toothbrush and avoid vigorous brushing to prevent further irritation and enamel wear. Adopting these practices can significantly reduce sensitivity and improve your overall oral comfort.
Achieving a Healthy Mouth With a Daily Oral Hygiene Routine
Maintaining a daily oral hygiene routine is essential for keeping your mouth healthy and preventing dental problems. You can ensure your teeth and gums stay healthy by incorporating effective brushing and flossing techniques, using mouthwash, cleaning your tongue, staying hydrated, eating a balanced diet, and visiting your dentist regularly. Advanced tips like using interdental brushes, oil pulling, choosing the right dental products, managing dry mouth, and treating sensitive teeth can enhance oral care. Remember, a healthy mouth is vital to your overall well-being, so prioritize oral hygiene in your daily routine.
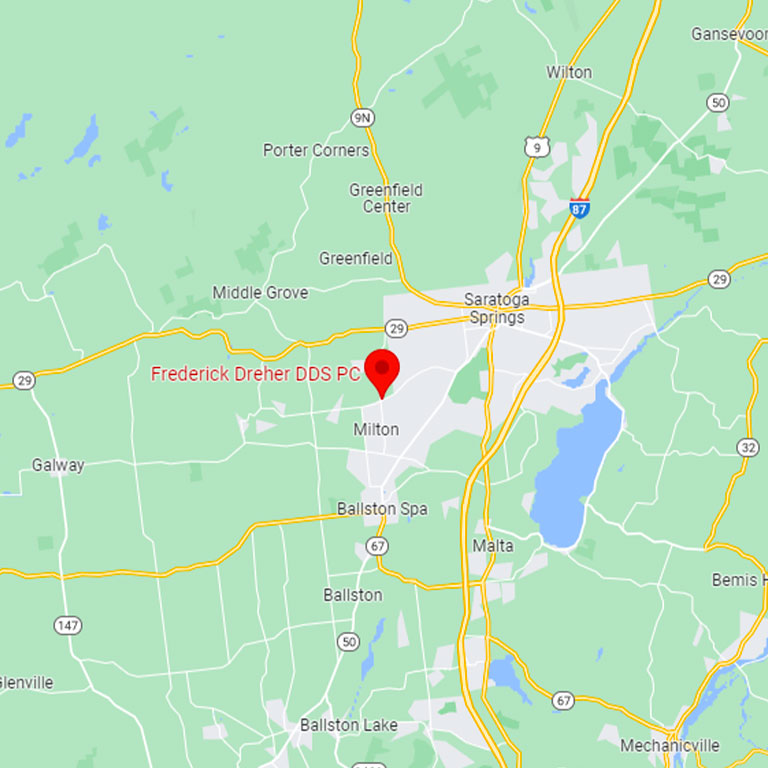
Visit our Frederick Dreher DDS PC blog for more in-depth tips and advice on maintaining oral health. Stay informed, and keep your smile bright and healthy!
























 Impact of Sedation in Dentistry
Impact of Sedation in Dentistry Preparing for Sedation at the Dentist
Preparing for Sedation at the Dentist
 Stages of Periodontal Disease
Stages of Periodontal Disease Periodontal Disease Treatments
Periodontal Disease Treatments