How to Treat Periodontal Disease
Addressing periodontal disease requires a comprehensive approach integrating professional dental treatments with diligent home care practices. It encompasses a spectrum of conditions, ranging from mild gum inflammation (gingivitis) to severe periodontitis, which can lead to tooth loss if left untreated. Any degree of gingivitis or severe periodontitis can be associated with periodontal disease, defined by infection and inflammation of the gums and tissues that support the teeth. Exploring the diverse treatment options is essential to managing this prevalent condition and maintaining optimal oral health effectively.
Professional dental treatments play a critical role in combating periodontal disease. These may include deep cleanings, also known as scaling and root planing, which involve removing plaque and tartar deposits from below the gumline to promote healing and prevent bacterial reattachment. Additionally, antibiotic therapy may be prescribed to control bacterial growth and reduce inflammation in the gum tissues. We will explore the comprehensive approach to treating periodontal disease and restoring oral health to understand more about this disease and the correct way to address the problem.
Understanding Periodontal Disease and Its Treatment
Periodontal disease, commonly known as gum disease, is a prevalent condition that affects the tissues surrounding the teeth. It begins with inflammation of the gums, known as gingivitis, and can progress to more severe forms if left untreated. If left untreated, periodontal disease can ultimately lead to tooth loss and other serious health complications. Professional treatments and conscientious at-home hygiene are combined to treat periodontal disease. People with this condition can effectively manage and reverse its progression by knowing its causes and available treatment options.
Eight Causes of Periodontal Disease
Periodontal disease affects millions of people worldwide and is a leading cause of tooth loss in adults. Understanding periodontal disease’s specific causes and contributing factors is essential for prevention and effective management.
1. Plaque Buildup
The leading cause of periodontal disease is the accumulation of dental plaque, a sticky film of bacteria that forms on the teeth. If plaque is not routinely removed by good oral hygiene habits like brushing and flossing, it can become tartar, or calculus, along the gum line. In addition to harboring more bacteria, tartar is difficult to remove and can irritate and inflame gums.
2. Poor Oral Hygiene
Poor oral hygiene practices, such as sporadic brushing and flossing, cause plaque to accumulate and stay on the teeth and gums. Plaque can cause gingivitis, inflammation of the gums, periodontitis, or more severe forms of periodontal disease.
3. Tobacco Use
Smoking and the use of tobacco products significantly increase the risk of developing periodontal disease. Regular smoking weakens the immune system’s response to bacterial infection, impairs blood flow to the gums, and hinders the healing process, making individuals more susceptible to gum disease.
4. Genetic Factors
Periodontal disease may be genetically predisposed to develop in some people. Specific genetic variations can influence the body’s reaction to bacterial plaque, raising the risk and severity of gum disease.
5. Systemic Health Conditions
Specific systemic health conditions can also contribute to the development and progression of periodontal disease. Diabetes and other illnesses impair the body’s defenses against infection, including gum disease. Other immune-compromising systemic diseases can also impact gum health.
6. Hormonal Changes
Fluctuations in hormone levels, such as those occurring during puberty, pregnancy, or menopause, can make gums more sensitive to gingivitis. Hormonal fluctuations can modify the body’s reaction to bacterial plaque, raising the risk of gum disease during these times.
7. Medications
Some medications, particularly those that reduce saliva flow or have side effects on gum tissues, can increase the risk of developing gum disease. Medications for heart problems, anticonvulsants, and antihistamines can all impact oral health and aggravate gum inflammation.
8. Poor Nutrition
A diet lacking essential nutrients, especially vitamins and minerals that support immune function and gum health, can increase susceptibility to periodontal disease. Gum inflammation is made worse by a diet heavy in sugary or starchy foods, which encourage bacteria growth and plaque formation.
Understanding the various causes and risk factors associated with periodontal disease is crucial for adopting preventive measures and seeking appropriate treatment. By implementing lifestyle modifications, professional dental care, and proper oral hygiene, individuals can mitigate the risk of developing periodontal disease and preserve the health of their teeth and gums. Preventive care and early detection depend on routine dental cleanings and examinations by professionals.
 Stages of Periodontal Disease
Stages of Periodontal Disease
As periodontal disease advances, it goes through different stages, each with its own set of symptoms and effects on oral health. Understanding these stages is essential for early detection, effective treatment, and prevention of complications.
Gingivitis
Gingivitis is the earliest stage of periodontal disease. Bleeding, swollen, and red gums are signs of gingivitis. Since the infection has not yet reached the bone and supporting structures, it is treatable with good oral hygiene and professional dental care.
Periodontitis
Without intervention, gingivitis can progress to periodontitis. In this stage, the infection spreads below the gumline, causing the gums to pull away from the teeth and form pockets. The bone and connective tissue that hold teeth in place can be broken down by bacterial toxins and the body’s immune system. Teeth may become loose with time and need to be extracted.
Understanding the stages of periodontal disease is essential for maintaining good oral health and stopping its progression. People can proactively seek out timely dental care and intervention by being aware of each stage’s telltale signs and symptoms. Appropriate care and strict oral hygiene can reduce the effects of periodontal disease and enhance general dental health and well-being.
Periodontal Disease Symptoms
Gum disease, another name for periodontal disease, can have a range of symptoms from minor to severe. Here are some common signs and symptoms to be aware of:
Gum Inflammation (Gingivitis)
The initial stage of periodontal disease, known as gingivitis, is characterized by visible signs of gum inflammation, including inflammation, redness, and tenderness. Additionally, gums can bleed readily, especially when brushing or flossing. Changes in the gums’ appearance, such as a shiny or puffed texture, can also be noticed.
Receding Gums
As periodontal disease progresses, gums may recede or pull away from the teeth. This may result in the gums changing color and exposing the tooth roots. Teeth may appear longer and become more sensitive due to receding gums.
Bad Breath (Halitosis)
Persistent bad breath, also known as halitosis, is a common symptom of periodontal disease. It often persists despite regular brushing. The odor is usually caused by bacteria in the mouth due to gum infection and inflammation.
Changes in Tooth Alignment or Bite
Advanced periodontal disease can significantly alter the bite or alignment of teeth. Teeth may move or loosen as the supporting bone and tissue deteriorate, which can alter how teeth fit together during biting and chewing.
Sensitive Teeth
Increased tooth sensitivity to hot or cold temperatures is another symptom of periodontal disease. The sensitive tooth roots become visible when the gums recede, causing this sensitivity. It’s possible to feel uncomfortable when eating or drinking.
Abscesses
In severe cases of periodontitis, abscesses may form around the teeth and gums. These are pockets of infection filled with pus and can cause localized swelling, pain, and tenderness. Abscesses require prompt dental attention to prevent further complications.
Recognizing these symptoms and seeking timely dental evaluation and treatment are essential for managing periodontal disease and preventing its progression. Regular dental visits and good oral hygiene practices can help detect gum disease early and minimize its impact on oral health.
 Periodontal Disease Treatments
Periodontal Disease Treatments
The treatment of periodontal disease varies depending on the severity of the condition. Here are several approaches commonly used by dentists and periodontists to manage and treat periodontal disease:
Professional Dental Cleaning (Scaling and Root Planing)
The initial step in treating periodontal disease involves a deep cleaning procedure called scaling and root planing. This procedure aims to help the gums reattach to the teeth by scaling (removing plaque and tartar) and root planing (smoothing out rough spots on the tooth roots).
Ozone Therapy
Ozone therapy is a revolutionary dental treatment that utilizes ozone gas to eliminate harmful bacteria, viruses, and fungi in the oral cavity. This non-invasive method not only disinfects but also promotes faster healing and tissue regeneration. Ideal for treating cavities, gum disease, and infections, ozone therapy offers a safe and painless alternative to traditional dental procedures.
Slide Analysis
Slide analysis of plaque identifies the specific bacteria present in the mouth. This detailed assessment helps tailor treatment solutions, sometimes including homemade toothpaste formulations. Understanding the exact bacterial composition allows for more effective and personalized dental car
Antibiotic or Antimicrobial Medications
Antibiotics or antimicrobial agents may be prescribed to help control bacterial infections associated with periodontal disease. These medications can be taken orally, applied directly to the gums, or placed into the periodontal pockets during scaling and root planing.
Surgery Interventions
In more advanced cases of periodontal disease, surgical interventions may be necessary to restore gum health and address damage to the surrounding tissues. Surgical procedures may include:
Flap Surgery
It is known as periodontal flap surgery or pocket reduction surgery. The surgery involves lifting the gums to remove tartar and smoothing damaged bone surfaces. It is a common procedure used to treat advanced stages of periodontal disease. During flap surgery, the gum tissue is gently lifted back to expose the roots of the teeth and the underlying bone.
Soft Tissue Grafts
It involves replacing receding gum tissue with tissue from another part of the mouth. During this procedure, tissue is taken from one area of the mouth, typically the roof of the mouth, and transplanted to another location where gum tissue is lacking.
Bone Grafts
It involves replacing damaged bone around the tooth roots to promote regeneration and stability. This procedure is often necessary for patients who have experienced bone resorption due to tooth loss, periodontal disease, or trauma. During a bone graft procedure, bone material is harvested from another part of the body or obtained from a donor source.
Maintenance and Follow-Up Care
After initial treatment, regular follow-up appointments with a dental professional are essential to monitor progress and maintain oral health. Periodontal disease can be prevented by practicing good oral hygiene at home, which includes brushing, flossing, and using mouth rinses with antimicrobial agents.
Lifestyle and Behavioral Changes
Making lifestyle changes such as quitting smoking and improving oral hygiene habits can significantly contribute to the success of periodontal disease treatment. Smoking cessation is significant as smoking can impair healing and increase the risk of periodontal disease progression.
Ongoing Periodontal Maintenance
Regular maintenance cleanings and exams by a dentist are often necessary for the long-term management of periodontal disease. These checkups help monitor gum health, spot any indications of disease recurrence, and avert further issues.
To treat periodontal disease effectively, a tailored approach based on each patient’s unique condition and needs is necessary. Early detection and intervention can preserve oral health and halt its advancement. Regular dental visits and open communication with your dental provider are key to successful periodontal disease management.
Home Care for Periodontal Disease
Home care plays a critical role in managing and preventing the progression of periodontal disease. Individuals suffering from periodontal disease can reduce inflammation, manage bacterial growth, and maintain healthier gums by implementing appropriate oral hygiene practices and lifestyle modifications. Here are essential home care strategies for managing periodontal disease:
Brushing
Brush your teeth at least twice a day using a fluoride toothpaste.
Flossing
Floss daily to remove plaque and food particles from between your teeth.
By understanding periodontal disease and its contributing factors, individuals can take proactive steps to prevent its onset or progression. Gum health preservation and maintaining a healthy smile depend heavily on early detection and prompt treatment. The management and prevention of periodontal disease largely depend on routine dental checkups and consistent oral hygiene practices.
Effective Treatment Options for Periodontal Disease
Treating periodontal disease requires a proactive and comprehensive approach that combines professional dental interventions with diligent home care practices. By understanding the causes and stages of gum disease and seeking timely treatment from a qualified dentist, individuals can effectively manage periodontal disease and prevent further complications such as tooth loss and systemic health issues. Remember, early detection and consistent oral hygiene are key to maintaining healthy gums and teeth for a lifetime.
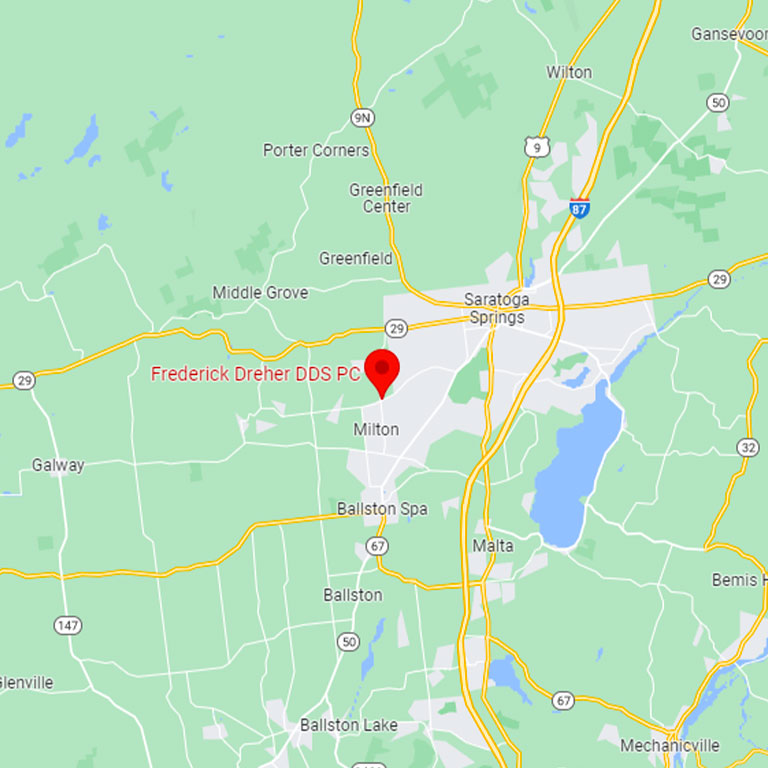
Take charge of your oral health today! Visit Frederick Dreher, DDS PC’s blog, for valuable insights and to learn more about our periodontal therapy services.





Leave a Reply
Want to join the discussion?Feel free to contribute!